ECMO Vs. VAD
Ventricular assist device (VAD) and extracorporeal membrane oxygenation (ECMO) are two similar temporary techniques to bridge cardiac therapy or transplants. In rare cases, they can also be a more permanent therapy for patients who are ineligible for transplants. ECMO systems typically bypass the heart entirely, taking deoxygenated blood from the IVC/SVC, oxygenating it through membrane filters externally, and pumping the oxygenated blood directly back into the cardiovascular system. ECMO systems can be V/V (venous to venous) or V/A (venous to arterial).

VAD systems assist the body by taking the load off of a ventricle and circulating blood at appropriate flow rates. Respiratory assist devices provide support by removing C02 or oxygenating blood to assist the lungs. All of these techniques require cannulation and often long-term 24/7 patient monitoring.
Choosing a Surgical Approach
The device that you’re testing typically dictates the surgical approach. We take into consideration the size and length of cannulas and cables, the desired indwelling anatomical location, and the blood volume or flow required among other requirements. ECMO and LVAD may require any one or a combination of the following surgical approaches:
- Thoracotomy (with or without graft)
- Jugular or carotid access
- Retroperitoneal access
- Femoral vein or artery access

Why wouldn’t you use femoral access?
Although it’s very common in clinical applications, femoral veins/arteries are less common in preclinical ECMO or VAD models for several reasons.
- The length of anatomy from the femoral vein/artery to the heart in large, four-legged animals is greater compared to humans and most devices would need to be custom-built for greater length (increased from 90–100 cm to 110 cm or greater)
- Once the animal is recovered, keeping the cannula/catheter in place is challenging at best, or impossible
- The angle of insertion may bend or break the cannula and often pinches the cannula at the access site

Note on the Use of Animals
Veranex is dedicated to the advancement of animal and human health. The animals at our Atlanta and Paris facilities are cared for with the highest respect and gratitude. We recognize that it is a privilege to work with these animals and believe that their lives have high value. We’re grateful for their sacrifice in helping to advance the medical field and improve outcomes for humans for years to come.
Species Selection: Unsuitable Models
Porcine Models
Although anatomically suitable for short-term acute or early feasibility studies, swine are not suitable for long-term ECMO or VAD studies. They’re difficult to restrain as tethering or normal restraints lead to rolling, scratching, or damage to the tubing/devices. Long-term restraints would require lifts/harnesses that restrict movement entirely or heavy sedation.
Canine Models
Canine anatomy is too small for the devices and, similarly to swine, they are difficult to restrain for long periods of time to prevent rolling/tangling in cables and external tubing.
Species Selection: Suitable Models
Ovine Models
Suffolk Crossbred sheep are approximately 50–80kg at the time of the initial procedure, which is a sufficient size and blood volume for most ECMO/VAD studies. They have a shorter body length, which can make the device placement easier relative to calves, but do not respond well to being separated from other sheep in isolation. Overall, they’re docile and tolerant of externally placed catheters/monitoring equipment but can be less accepting of tethering and are prone to being skittish while being handled if not acclimated properly.
Bovine Models
Beef/Dairy Cross calves are 70–90kg at the time of the initial procedure. Their larger vascular anatomy allows for convenient cannula placements and their larger blood pool allows for more blood sampling. Juvenile calves can have some initial illnesses or acclimation stress during transportation but are typically docile and tolerant of externally placed catheters and monitoring equipment.
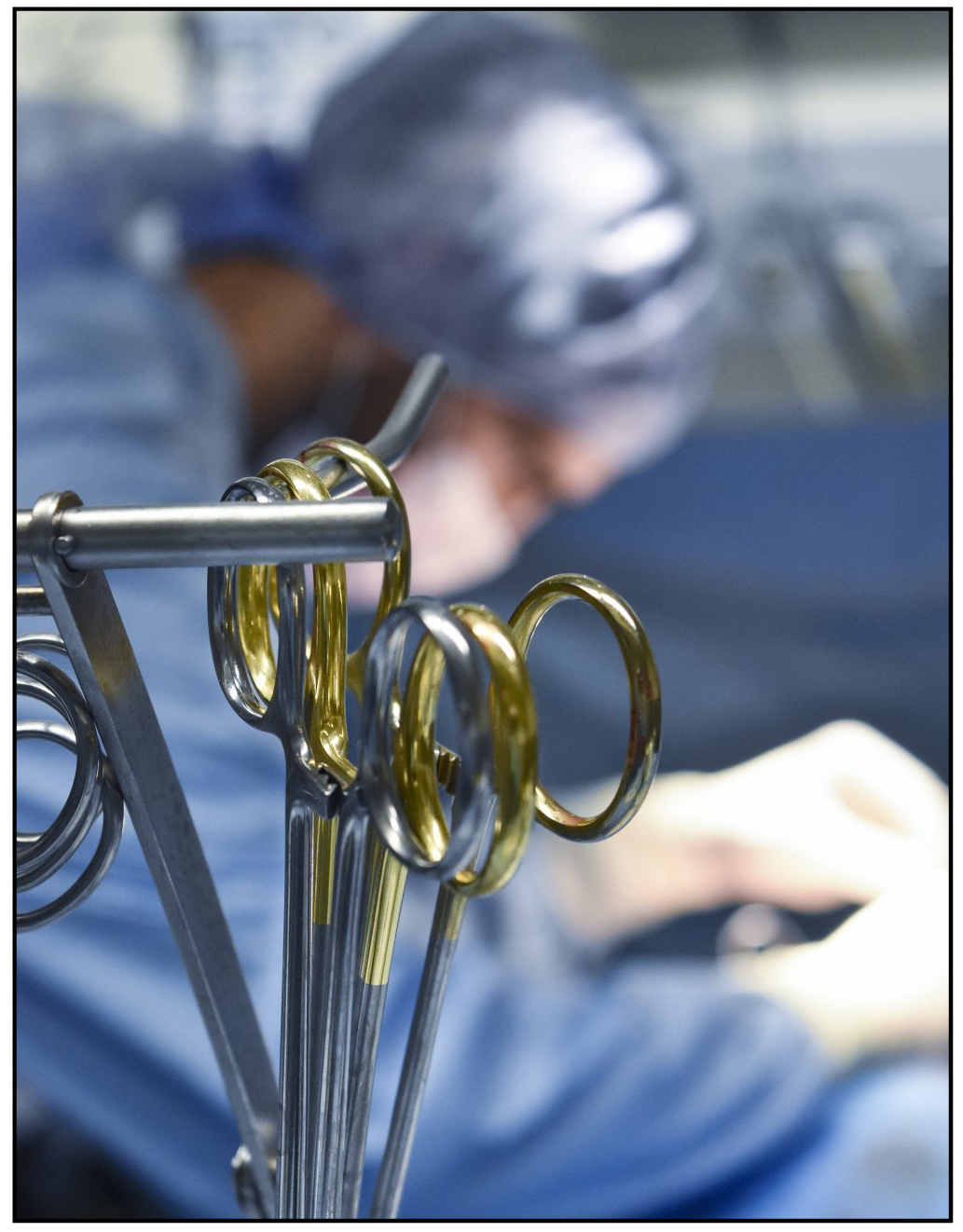
Implant Procedures
Our surgical team can perform the entire implant operation with assistance from sponsor engineers priming their ECMO/VAD circuit and controller. Our team is experienced in surgical placement via thoracotomy, jugular, carotid access, and retroperitoneal approaches.
Indwelling Venous Line
We place the indwelling venous line at the right or left jugular vein (typically a Hickman 9.6 Fr). We typically shorten the length and puncture additional holes near the tip to prevent suctioning to the wall during blood draws. This line is usually left in throughout the duration of a study and is used to administer the heparin CRI and drugs as well as obtain blood samples for ACT, blood gases, and blood tubes.
Animal Recovery
Before leaving surgery, the animal is placed sternal and needs to be breathing independent of a ventilator. They’re then transported to the vivarium with a circuit connected and pump running, typically on a mobile cart behind a lift table. The animal is carefully moved into the stanchion while being mindful of the tubing and cables. From there, the animal is placed in an individual pen that prevents the animal from being able to turn around and is designed to keep the tubing from becoming tangled. The animal is monitored by veterinarian staff 24/7 for the duration of the study, which requires constant ACT checks and heparin drip titration. Our team vigilantly checks and records the animal’s vital signs and behavior. We also perform SOAP exams, TPR, blood gases, and collect blood tube samples regularly.
Anticoagulation
Most ECMO/VAD devices require some form of anticoagulation. Using Heparin CRI (100,00 U / 1L bag saline) carefully titrated over time to bring ACT within a predetermined range has been our most successful method. We’ve also attempted other anticoagulation such as Clopidogrel/Aspirin and warfarin with minimal success. ACTs are checked every four hours when within range and every one to two hours when outside or trending outside of range to minimize sampling.
Anticoagulation
Measuring
Abbott I-Stat
- Cartridge-based system requires <1 ml per sample
- Our preferred method for ICU-style studies
Hemochron Response
- Spinning tube-based system that requires ~3 ml of blood per sample
- In our experience, I-Stat generally records slightly lower ACT values comparatively, but has much more consistent values
- The hemochron system records slightly higher values, but can vary in value range more dramatically from sample to sample
Target Range
This is defined in the GLP protocol. There are two common methods: 1) Set the range to 1.5x to 2.0x baseline ACT value for each animal
- Specifically set for each animal
- Highly dependent on initial baseline reading
- Makes tracking ranges between multiple animals more challenging
2) Set range (e.g. 200 seconds to 350 seconds)
- Makes tracking ranges simpler between animals
- Not specifically tied to individual animal baselines
Other In-Life Parameters
SOAP Exams: Also known as Subjective, Objective Assessment Plans, this includes a comprehensive veterinary exam of the animal. It’s typically done daily initially, and with decreasing frequency over the course of the study if the animal is healthy and doing well. Device Parameters: This includes pump flow, motor current, pressure values, etc. It’s performed at regular intervals (e.g. 8, 12, or 24 hours). Blood Gases: i-Stat CG8+ cartridges measure values such as SPO2, nitrogen, glucose, potassium, etc. This is performed daily initially and with decreasing frequency over the course of the study if the animal is healthy and doing well. Hemocrit: This is measured via spin of capillary tubes. It indicates anemia or hemolysis and is performed daily. Plasma-Free Hemoglobin: This is measured via our HemoCue system or via Spectrophotometer. It indicates hemolysis and is performed daily. Clinical Pathology: We capture CBC, serum chemistry, fibrinogen, and D-dimer. This is performed daily initially and with decreasing frequency over the course of the study if the animals are healthy and doing well.
Outcomes
In our experience, with proper maintenance and no major health concerns, animals can typically be maintained with 24-hour care for 7–21 days. Although some studies have gone as long as 30 days, anticoagulation therapy along with continuous ECMO/VAD therapy tends to have more complications after day 14 and beyond. Acceptable mortality rates need to be considered when going for extended periods of time as there are limitations and clinically adverse events expected in both ovine and juvenile bovine models.

- Requires 42, 12-hour shifts with 4 staff members per shift
- Totals a minimum of 2,016 skilled labor hours while maintaining GLP compliance and ensuring the welfare of the animals
- Remember to add in time for a study director, veterinarian, quality assurance, etc.
Potential Clinically Adverse Events
1. Anemia – due to prolonged circuit therapy, numerous blood samples, or anticoagulation
- Monitored by manual hematocrits, clinical pathology, and plasma-free hemoglobin
- Reducing or halting heparin CRI can often reverse some anemia, but increases the risk or clotting
- Blood donation from a naive animal, if allowed, in protocol and an emergency condition can be helpful
2. Hemorrhaging/Hematomas – at vascular access sites
- More common in jugular or carotid access sites with anticoagulation running compared to retroperitoneal or thoractomy
- Treatable in most cases with pressure bandages or manual draining
3. Infections
- More common in retroperitoneal or thoractomy access sites
- Despite best efforts, these surgical accesses are not 100% sealed to bacterial ingress along the tubing/drive lines
- Access sites are cleaned daily
- Temperature and SOAP exams are typical first signs
- Antibiotics are typically given for ~3 days post-operatively
- Antibiotics could be given continuously, but calves and sheep with prolonged antibiotics can have digestive issues and the study should not mask potential GLP safety issues by blanketing antibiotics without clinical indicators
4. Clotting – in the tubing, oxygenator, pump, or other parts of the circuit
- Although certain parts may be replaceable, some are not or would be considered failed endpoints by the GLP protocol
- Some fibrinous growth in tubing and oxygenator is often expected and typical as long as it does not hinder or occlude flow and does not break off as it would be later found in downstream organs
- Thrombus – resulting in stroke, cardiac arrest, or pulmonary embolism
- Very few treatment options, typically resulting in an early mortality or early termination
5. Acute Interstitial Pulmonary Emphysema – also known as interstitial pneumonia (AIP)
- Common cause of sudden respiratory distress in cattle
- Sudden onset of clinical signs with minimal coughing and severe difficulty breathing similar to an asthma attack
- Affected animals often die despite supportive treatment
- Bubble-like appearance of lungs is an indication at necropsy
